Nurs Econ. 2015;33(1):8-12.
Abstract and Introduction
Introduction
Unlike most other countries, there have long been multiple routes toward becoming a registered nurse (RN) in the United States. For decades, RNs have been prepared via three main pathways; a 2-year associate's degree program, a 3-year hospital-based diploma program, and a 4-year baccalaureate program leading to a bachelor's degree in nursing (BSN). Diploma programs have all but disappeared, leaving roughly equal numbers of RNs obtaining their initial preparation toward becoming an RN via the associate's degree programs (ADN) or the BSN. According to the National Sample Survey of Registered Nurses (n.d.), of RNs completing their initial RN education between 2005 and 2008, approximately 3% were prepared via a diploma program, 57% via an ADN, and 40% via a BSN.Not apparent in those figures, however, is a recent apparent shift in basic entry nursing education away from the ADN and toward the BSN (Buerhaus, Auerbach, & Staiger, 2014). Beginning roughly a decade ago, the American Nurses Credentialing Center (2013) began designating hospitals as Magnet® institutions based on certain quality and other benchmarks, one of which is that by January 2011, 75% of nurse managers must have at least a BSN. Then, building on a series of research studies over the last decade beginning with Aiken, Clarke, Cheung, Sloane, and Silber (2003) who indicated the risk of inpatient mortality is lowered in hospitals employing a greater share of BSNprepared RNs, the Institute of Medicine (2010) recommended 80% of RNs be prepared at the BSN level by 2020. States and institutions appear to have taken up the call; by 2014, 80% of California hospitals require new RN staff to have a BSN (Bates, Chu, Keane, & Spetz, 2014).
These forces may be having important implications for the nursing workforce. Kovner, Brewer, Fatehi, and Katigbak (2014) recently comparing a cohort of roughly 1,000 newly licensed nurse graduates (2010–2011) and found 82% of new BSN graduates were em ployed in hospitals within 18 months of graduation compared to 67% of ADN graduates. In contrast, in an earlier similar cohort graduating in 2004–2005, 83% of new ADN graduates found hospital jobs in the same time frame after graduation. Kovner and colleagues (2014) cited "anecdotal re ports that hospitals are preferentially hiring RNs with a BSN and that if they do hire associate's de gree grad uates, they are requiring those nurses to get a BSN within a specified period" (p. 32). In fact, in 2010, while there were roughly 80,000 ADNs and 50,000 BSN nursing degrees awarded among newly licensed RNs, another 22,000 RNs completed RN-to-BSN programs, converting their ADN preparation to a BSN (Bates & Spetz, 2012).
With the exception of the study by Kovner and associates (2014), however, it is unclear if this apparent preference for BSN-prepared RNs has markedly changed the labor market outlook for a RN who has completed an ADN. These programs have proliferated (along with BSN programs) in the largest expansion of undergraduate nursing education in recent history (Auerbach, Buerhaus, & Staiger, 2013). If this preference for BSN-prepared RNs is truly widespread and universally accepted, one might expect ADNs to be shifting to other employment settings and/or receiving lower wages. In this article, recent employment and earnings data from the American Community Survey is examined to determine whether any of these expected changes are occurring in the nurse labor market.
Data and Methods
Data
The primary data used in the analysis are from the American Community Survey (ACS) (King et al., 2010). The ACS, which began reporting data in 2001, is modeled after the long form of the decennial census (U.S. Department of Labor, 2014) and obtained responses from approximately 12,000 RNs each year from 2001 to 2004 and roughly 30,000 RNs per year thereafter (after the sampling frame was expanded). The ACS identifies RNs by allowing respondents to select their occupation and obtains additional data on respondents' age, educational level, income, industry sector, and other demographic information and has been used extensively by our team to analyze the nursing workforce (Auerbach, Buerhaus, & Staiger, 2011).Data on RNs between the ages of 21 and 64 were used in this analysis for the years 2003–2013; RNs reporting working fewer than 30 hours in a typical week were recorded as 0.5 full-time equivalents (FTE). RNs reporting a master's level of education or higher were excluded to focus specifically on RNs working as an RN (rather than as a nurse practitioner, for example, which requires a BSN typically followed by an advanced degree). Although the ACS data were first collected in 2001, this analysis begins with 2003 because of a change in the education questions between 2002 and 2003. The final sample included 217,815 RNs across all years.
Identifying Nursing Education
To our knowledge, the ACS has not been used to distinguish ADNs from BSNs in peer-reviewed research. ACS respondents report whether their highest level of education completed is an associate degree, a 4-year college degree, or one of various types of higher degrees such as master's or doctorate. As a simplification, we classified all RNs reporting a bachelor's degree as a BSN-prepared RN and RNs with less-reported education as ADN-prepared RNs (RNs with at least a master's degree were removed from the sample). The reported degrees in the ACS are not nursing-specific, although respondents could indicate a field for baccalaureate degrees starting in 2009. (This information was not used for purposes of consistency with the time period before 2009.) Thus, RNs prepared with diploma degrees (of which there are very few in recent years) would likely be unsure how to classify their education in the ACS. More importantly, RNs with bachelor's degrees in non-nursing fields but no higher than an ADN in nursing would likely select a bachelor's degree as their highest degree and we would be unsure whether they were a BSN or ADN-prepared RN.To validate the ACS-based assignments, data from the National Sample Survey of Registered Nurses (NSSRN) from 2008 were analyzed and compared to the reported education of RNs to the educational categorization of RNs from the ACS in that same year. The NSSRN, discontinued in 2008, asked RNs directly about their initial and any subsequent nursing degrees as well as other non-nursing degrees. In 2008 NSSRN data, just 5% of respondents had a non-nursing baccalaureate degree but also a highest nursing preparation of an associate's degree. (Another 8% of RNs had baccalaureate degrees both in nursing and in a non-nursing field, but these individuals would be correctly classified in the ACS as BSN-prepared RNs). Overall, after excluding all RNs with a master's degree or higher, our assignments in the ACS yielded 41.3% of RNs with an ADN as their highest nursing degree and 58.7% with a BSN. This is similar to the comparable figures of 43.8% and 56.2%, respectively, in the NSSRN. Other characteristics of ADN-prepared RNs and BSN-prepared RNs were compared between both surveys – patterns were identical. In both surveys, the BSN-prepared RNs were more likely to be male, non-White, unmarried, higher household income and nursing income, foreign educated, and working in hospitals (data available upon request).
Other Labor Force Measures
Labor market outcomes were recorded from direct questions asked in the ACS survey. Unemployed RNs were defined using variables constructed within the ACS based on detailed questions concerning the respondent's employment status (looking for but unable to find employment). Respondents were asked to report their income from wages and salaries in the previous 12 months; this dollar amount was used as an estimate of earnings from nursing employment. Earnings figures were reported only for RNs who work full time, as defined by those reporting working more than 30 hours per week. Finally, all ACS respondents were asked to identify their industry setting from a list that we consolidated into hospitals, offices of physicians and other health professionals, nursing homes and other long-term care settings, other health care settings, and settings unrelated to health care.To make estimates representative of the U.S. noninstitutionalized population, observations were weighted by sampling weights provided by the ACS. In several instances, statistical significance of differences between ADN and BSN RNs are reported. These tests were conducted using two-tailed tests, with 0.05 as the level governing statistical significance.
Results
Differences Between ADN-prepared RNs and BSN-prepared RNs
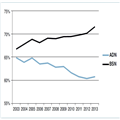
Differences in the rate of unemployment among both types of RNs are shown in Figure 1. Though historically quite low, the unemployment rate has diverged between RNs prepared with a BSN and those with an ADN in recent years.
Figure 1.
Unemployment Rate of RNs, by Ultimate Degree Type, 2003–2012
The trends in FTE employment suggest a fairly dramatic divergence in hospital employment by type of basic nursing education (see Figure 2 and Table 1). In 2003, a similar percentage of RNs with each degree type worked in hospitals. A few years later, a gap in hospital employment had started to materialize, and, by 2013, more than 10 percentage points separated the two groups, with 72% of BSN graduates employed in hospitals compared to 61% of RNs whose highest degree was an ADN. These data are consistent with a growing preference for BSN-prepared RNs on the part of hospitals.
Figure 2.
Percent of Full-Time Equivalent RNs Employed in Hospitals By Ultimate Degree Type, 2003–2013
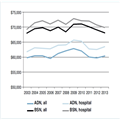
Finally, trends in overall earnings and earnings among hospital-employed RNs over the same time period are shown in Figure 3. In contrast to the trends shown in Figures 1 and 2, the data shown in Figure 3 do not indicate a divergence over the 10-year time period. If anything, the wage gap between ADNs and BSNs, which has been relatively constant over the last decade at roughly $10,000 for RNs in hospital and other settings, has shrunk slightly in the last 2 years.
Figure 3.
Overall and Hospital-Employed Earnings of Full-Time Equivalent RNs by Ultimate Degree Type, 2003–2013
NOTE: Earnings figures exclude those of RNs working fewer than 30 hours per week.
NOTE: Earnings figures exclude those of RNs working fewer than 30 hours per week.
Discussion
In two of three labor market outcomes analyzed using data from the ACS, there was a divergence of the experience of AND-prepared RNs compared to BSN-prepared RNs. ADNs are more likely to be unemployed (though unemployment rates are still extremely low) and increasingly less likely to work in hospitals than their BSN counterparts. These findings are consistent with hospitals' expressing a preference for BSN graduates in recent years. On the other hand, although BSN earnings are greater than ADN earnings in every year of the sample, there does not appear to be a widening divergence in the earnings between BSN and ADN-prepared nurses.As with any labor market evaluation, it is difficult to discern whether the observed differences in unemployment rates and hospital employment by level of nursing education reflect the RN's education itself, or whether other characteristics of the RN who may obtain different degrees could also be related to these labor market outcomes. With regard to the latter possibility, it is unlikely in the short time frame of these observations (2003–2012) that characteristics of RNs who obtained an ADN or a BSN have changed substantially. Rather, the timing of the divergence in unemployment rates between ADN and BSN-prepared RNs, and to some extent, the increased employment of BSNs in hospitals found in this analysis, appears to have occurred several years before the 2010 Institute of Medicine (IOM) report The Future of Nursing: Leading Change, Advancing Health was released. In the middle part of the decade, hospitals were becoming aware of a growing body of evidence indicating the association of lower mortality and higher BSN-educated RNs. Moreover, in 2008 the Centers for Medicare & Medicaid Services and several states began to link hospital payment to performance on avoidable inpatient outcomes, some of which were sensitive to nurse staffing (Kurtzman & Buerhaus, 2008) Later, the IOM (2010) report was released. The IOM emphasized the need for a more highly educated nursing workforce, and its wide dissemination more than likely provided "tipping point" information that influenced employers' decisions to prefer the more highly educated BSN.
Finally, it should be noted our estimates of RNs by level of educational preparation are imperfect. As noted previously, the educational categories in the American Community Survey are not designed specifically to identify nursing education. Also, individuals in the ACS are identified as nurses by their answers to the occupation questions. Yet, in both cases, findings from the ACS have been validated against data from the NSSRN and workforce and educational estimates are very similar.
Policy Implications
The IOM set a goal of 80% of newly graduating RNs having a BSN by 2020. This call has been echoed by others who have suggested a BSN-level preparation is needed for the increasing complexity of care (American Association of Colleges of Nursing, 2014). Supported by the Affordable Care Act, health care delivery organizations are placing increasing emphasis on quality metrics, care coordination, population health management, and prevention and education. Accountable Care Organizations, expanding rapidly in the last several years, have strong financial incentives to manage care of their enrollees. These organizations seek to reduce total costs and improve quality by requiring health care professions to eliminate care duplication, coordinate and manage care received at home and among fragmented providers, and reduce hospitalization.Our results indicate, as did Kovner and colleagues (2014), ADN-prepared RNs appear to be experiencing diverging labor market outcomes from BSN-prepared RNs. Yet, at the same time, there has been a rapid increase in ADN educational programs over the last 10 years (Buerhaus et al., 2014). This growth may be helping to fill what would otherwise be a potential new nursing shortage as the baby boomer RNs begin to exit the workforce? Even if ADN-prepared RNs are not always finding the hospital positions some of them expect upon entering nursing school, the widespread availability of RN-to-BSN programs provides a relatively easy step for conversion to a BSN. Ultimately, it is unclear whether ADNs are shifting away from hospital settings out of necessity because hospital jobs are unavailable, or if their skill set is better suited for less-acute nonhospital patients.
Thus, the increasing percentage of ADN-prepared RNs employed in nonhospital settings, just as demand for RNs in these settings appears to be increasing, is a finding that requires close monitoring (Spetz, 2014). Most studies of care outcomes differences between ADNs and BSNs have focused on hospital care; there is no evidence to suggest any quality differences in nonhospital settings. ADN programs may find it in their interest to specialize in, and focus on, the kinds of skills increasingly critical to enhanced ambulatory settings such as care coordination, communication, teamwork, population health, and education and prevention (Pittman, 2014). Ultimately, a robust, integrated, complex and efficient health care system requires a diverse nursing workforce and the schools that prepare nurses for this new world ought to anticipate these needs and graduate nurses with the skills and competencies required.